
Positive Pregnancy Test but No Baby on Ultrasound: Understanding Your Results
Receiving a positive result on a pregnancy test can fill you with a mix of joy and anticipation.

The risks of having a private ultrasound scan
On This Page: As a sonographer with two decades of experience in both the National Health Service (NHS)

Cancer Screening and the Role of Ultrasound
Cancer Screening: Why It Matters Cancer screening is a proactive health measure that identifies cancer before symptoms appear.

Can you see cancer in the abdomen with an ultrasound?
Detecting cancer early significantly increases the chances of successful treatment, which is why medical imaging plays a crucial

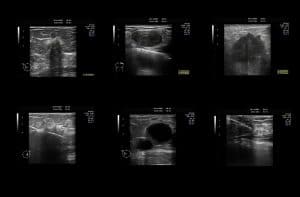
Ultrasound Scan
Are you having an ultrasound scan? Have you got questions? We have the answers.

Understanding Sound: From Physics to Medical Applications
Sound plays a fundamental role in our communication, entertainment, and understanding of the world. At its core, sound

No heartbeat at 6 weeks
Table of Contents Pregnancy is a period of significant anticipation and concern, especially regarding the health and development

The Benefits of Early Pregnancy Scans at a Private Clinic
Expecting parents know that early pregnancy scans are an important part of prenatal care, but many are unaware

How Private Ultrasound Can Help with Pregnancy Monitoring
Table of Contents Pregnancy is a journey filled with anticipation and a myriad of emotions. As expectant parents
Interpreting Your Follicular Tracking Scan Results
Follicular tracking scans, also known as fertility monitoring scans, are an important part of fertility treatments like IVF
Benefits of Follicular Tracking for IVF Treatments
In vitro fertilization (IVF) is a complex process that involves carefully tracking a woman’s ovarian follicles and hormonal
Understanding the Basics of Follicular Tracking
Follicular tracking, also known as follicle monitoring, is an important part of fertility care and treatment. It involves
Polycystic Ovary Syndrome (PCOS) and the Role of Follicular Scans
Polycystic ovary syndrome (PCOS) is a common hormonal disorder that affects women of reproductive age. It is characterized
The Role of Ultrasound in Fertility Treatments
Ultrasound imaging has become an integral part of fertility care and treatment. From initial fertility assessments to monitoring
The Role of Breast Ultrasound in Monitoring Breast Implants
Breast implants are a popular cosmetic surgery procedure that can enhance breast size and shape. However, like any
Testicular Ultrasound
Table of Contents Testicular ultrasound, also known as scrotal ultrasound, is an important imaging modality used to evaluate

Which is the most popular birthing hospital in London in 2023-2024
Are you trying to decide which is the best maternity hospital in London? Find out what other pregnant women have chosen.
The Role of Breast Ultrasound in Early Detection of Breast Cancer
Breast ultrasound plays a vital role in early detection, helping to distinguish between solid lumps and fluid-filled cysts
Breast Ultrasound for Women Under 40 – What You Need to Know
Ultrasound (US) is a safe and widely-used diagnostic method that has become the go-to alternative for mammography in
Understanding Breast Cysts and How Ultrasound Can Help
Breast cysts are fluid-filled sacs that form within the breast tissue. They’re most common among women between 30-50
The Difference Between Screening and Diagnostic Breast Ultrasounds
Breast cancer is one of the most common cancers affecting women worldwide, and early detection is key to
What Are the Benefits of a Private Testicular Ultrasound?
A testicular ultrasound is a non-invasive diagnostic imaging procedure that uses high-frequency sound waves to create images of
The Role of Breast Ultrasound in Diagnosing Breast Cancer
Introduction Breast cancer is a significant health concern for women worldwide, and early detection is vital for successful

Scanning the Horizon Exploring the Expansive Applications and Future of Ultrasound Technology
Ultrasound technology, a cornerstone of modern medical diagnostics, has evolved significantly since its inception. The foundational principles for
The Importance of Regular Breast Self-Examinations and Ultrasound Screening
Early detection of breast cancer is essential for improving mortality rates. Screening for this disease includes clinical breast
When to Get a Testicular Ultrasound
Ultrasound imaging of your testicles (also referred to as a sonogram) utilizes reflected sound waves to produce pictures
Private Ultrasound and Your Privacy: What You Need to Know
Ultrasound scans during your pregnancy are an invaluable way to learn more about your unborn child and can
Using Medical Ultrasound for Abdominal Conditions
Abdominal ultrasound is used to diagnose and monitor conditions in the abdomen, such as liver disease, gallstones, and
Private Ultrasound Scans for Fertility and Reproductive Health
Ultrasound is a non-invasive procedure that works by sending sound waves directly at your internal organs and detecting
Understanding the Differences Between Breast Ultrasound Mammogram and MRI – A Comprehensive Guide
Thanks to advances in medical technology, breast cancer and other breast issues can now be detected at an
The Importance of Early Detection in Breast Health. How Breast Ultrasound Can Help
Early detection saves lives, especially when it comes to breast health and the potential risks of breast cancer.

What are the advantages of a private breast ultrasound scan?
Breast ultrasound scans are an essential diagnostic tool in the field of medical imaging. These scans are used

What are the most common reasons for a breast ultrasound scan
Breast ultrasound is a non-invasive and painless imaging technique that uses high-frequency sound waves to create images of
Morning Sickness in Pregnancy
Pregnancy is almost synonymous with morning sickness. It is the most common disorder of early pregnancy, affecting up to 85%
Understanding Your Ultrasound Results: A Guide for Patients
Ultrasound imaging, or sonography, is a non-invasive medical diagnostic procedure that uses ultrasonic sound waves to create images

Comparing NHS vs Private Ultrasound What’s the Difference
Ultrasound is an imaging technique that uses sound waves to create a real-time image of the inside of

Preparing for Your Ultrasound: What to Expect and How to Get Ready
What is an Ultrasound? An ultrasound is a diagnostic medical test that uses high-frequency sound waves to produce

The Importance of Private Ultrasound Scans in Cancer Detection and Treatment
Private ultrasound scans are an important and invaluable resource in cancer detection and subsequent treatment. Ultrasound techniques provide

Ultrasound for Gynaecological Conditions: A Patient’s Guide
Ultrasound is a type of imaging that uses sound waves to create images of organs inside the body.

Ultrasound for Ovarian Reserve
Ultrasound in the form of pelvic scan is one of the first tools employed to evaluate a woman’s

Private Ultrasound Scan NHS
If your doctor has referred you to your local NHS hospital for an ultrasound scan, you are probably

Ultrasound And Its Top 9 Uses
Ultrasound imaging, also known as sonography or diagnostic medical sonography, has become an indispensable tool in modern medicine.

What is obstetric ultrasonography?
What is obstetric ultrasound? Obstetric ultrasonography refers to the deployment of ultrasound technology in the health evaluation of

Symptoms Of Ovarian Cysts
The symptoms of ovarian cysts are much more common in today’s society than people like to admit. What Are

Understanding pelvic ultrasound reports
Pelvic Ultrasound Results Explained. If you had a pelvic ultrasound scan and you are reading your ultrasound report
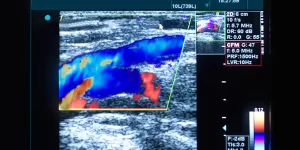
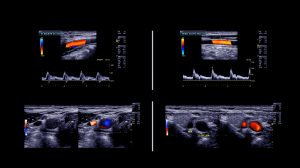
Doppler Ultrasound Imaging
You have probably wondered what are the red and blue colours you are seeing on the screen during

Early Pregnancy Scan. Your Questions answered
What is an Early Pregnancy Scan? The early pregnancy scan also called viability scan is an ultrasound test used in

Thyroid Ultrasounds: 5 Common Questions
What is a thyroid ultrasound? Ultrasound imaging, also called ultrasound scanning or sonography, involves the use of a

Pregnancy Spotting – What Causes Vaginal Spotting During Pregnancy?
Bleeding or spotting in early pregnancy can be very worrying, causing many pregnant mothers sleepless nights as bleeding

Understanding Medical Image Techniques
Medical image technology can mean the difference between a complex and uncertain diagnosis and a concrete assurance of

Pregnancy Ultrasound FAQs
All mother to be are offered pregnancy scans resulting in pregnancy ultrasound being one of the most common

Pelvic Ultrasound FAQs
The pelvic ultrasound is a diagnostic scan exam to evaluate the organs and structures within the female pelvis. The pelvic scan will

FAQ’s about International Ultrasound Services
Do I need a doctor’s referral, or can I self refer for a private ultrasound scan? Yes, you

Abdominal Ultrasound FAQs
Abdominal ultrasound is a type of imaging test used to look at organs in the upper abdomen, including

The Interesting Past of Notting Hill
The International Ultrasound services clinic is located only a few minutes walk from Notting Hill Gate Underground Station.

Why you Should be Undergoing Regular Medical Imaging Screening Tests
The introduction of affordable and convenient medical imaging services together with government and charity-led initiatives to raise awareness
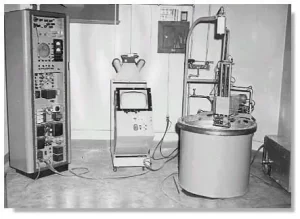
History of Ultrasound
Everyone is aware these days of the use of ultrasound in medicine, although most people will associate ultrasound

The Transvaginal Ultrasound Scan
Table of Contents Ultrasound imaging is a fundamental tool in medical diagnostics, offering a non-invasive glimpse into the

Why you should use a reputable ultrasound clinic for your scan?
There have been multiple reports through time in the media about the failings of private ultrasound providers resulting
Ultrasound for Cancer Screening – Questions and Answers
Ultrasound helps doctors look for tumours in certain areas of the body that don’t show up well on x-rays.

6 week Pregnancy Scan
Table of Contents Congratulations on your pregnancy and welcome to the world of baby scans. The 6 weeks

What is a Private Scan
Are you looking to book a private scan? We answer your most common questions.

Early Ultrasound for Determining Miscarriage
Miscarriage is very common in the first trimester of pregnancy and ultrasound is the diagnostic modality of choice to diagnose or exclude miscarriage

Use of Portable Ultrasound Equipment for at Home Pregnancy Scanning
Ultrasound is used during pregnancy to check the baby’s development and to help pick up any abnormalities. Ultrasound

Pregnant Women Allowed Partner Support at All Times
According to the latest NHS guidance you can now bring a partner with you at your maternity appointments

Why you should book a private ultrasound scan instead waiting for the NHS during the Covid-19 era
International Ultrasound Services offers private ultrasound in a convenient central London location. This private scan service is offered to patients

Baby Loss Helplines
The Lullaby Trust (formerly FSID the Foundation for the Study of Infant Death) Bereavement Helpline: 0808 802 6868 lullabytrust.org.uk The
COVID-19 Adjustments to Ultrasound Practice
How we try reduce the spread of Covid-19 cross infection.

7 week Baby Ultrasound Scan
Table of Contents It is quite common for our London pregnant couples to have their first pregnancy scan at around 7 weeks of

8-12 weeks Pregnancy Scan
Your eight-week private ultrasound scan can be an exciting and apprehensive moment. If this is your first pregnancy ultrasound you will be

Ultrasound Scans in Pregnancy
Pregnancy Ultrasound Scan A pregnancy ultrasound is the most widely used medical imaging method for viewing the foetus

Our most Frequent Pregnancy Scans
The pregnancy scans offered by the NHS might not always be enough to offer the reassurance that the pregnancy is
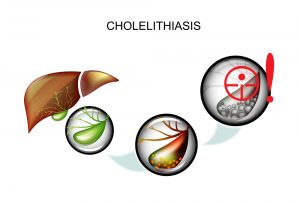
Abdominal Ultrasound Scan for Gallstones
The private abdominal scan is one of our most popular examinations. Upper abdominal pains that can be caused by calculi
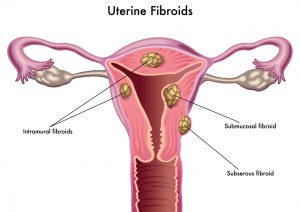
Ultrasound for Uterine Fibroids
What are fibroids Fibroids are benign (Non-cancerous) growths that develop from the muscle tissue of the uterus. Although their

Pelvic Infections: Causes and Prevention
Pelvic Infections or Pelvic Inflammatory Disease (PID), is a term used for infection of Pelvic organs i.e the

Urinary Tract Infection in Women – Causes, Symptoms and Prevention
Urinary Tract Infection (UTI) is defined as the infection of any part of the Urinary system i.e. the

Ectopic Pregnancy Ultrasound Scan
Ultrasound imaging is the first line of tests performed when ectopic pregnancy is suspected.
Assessment Cycle or Tracking Cycle
What is a Tracking Cycle? We use a ‘Tracking Cycle or Assessment cycle’ to check that the orderly

Ultrasound for Common Urologic Conditions in Both Men and Women
The urinary tract ultrasound or US Urinary tract is the primary imaging modality in the investigation of the urinary tract

Testicular Cancer: Symptoms, Diagnosis, Treatment, Prognosis
Testicular Cancer Ultrasound The testicular ultrasound is one of our most common private ultrasounds in London for men to
Vascular Diseases
One of the most dangerous medical conditions existing in the world today is that of vascular disease. While it can

Symptoms of Thyroid Cancer
The thyroid ultrasound scan is one of the most common private ultrasound scans in London. It is very common to identify thyroid

Understanding 2D, 3D and 4D pregnancy ultrasounds
If you’re expecting a baby, you can most certainly expect a baby ultrasound scan. In the UK the

Medical Sonographer
Information about the healthcare professional who is most likely to perform your ultrasound examination.

The Thyroid – Function and Pathologies
What is the Thyroid? The thyroid gland is the biggest gland in the neck. It is situated in the anterior






