Ultrasound in the form of pelvic scan is one of the first tools employed to evaluate a woman's fertility by counting the number of antral follicles to evaluating the ovarian reserve and quality of eggs..
What are Follicles?
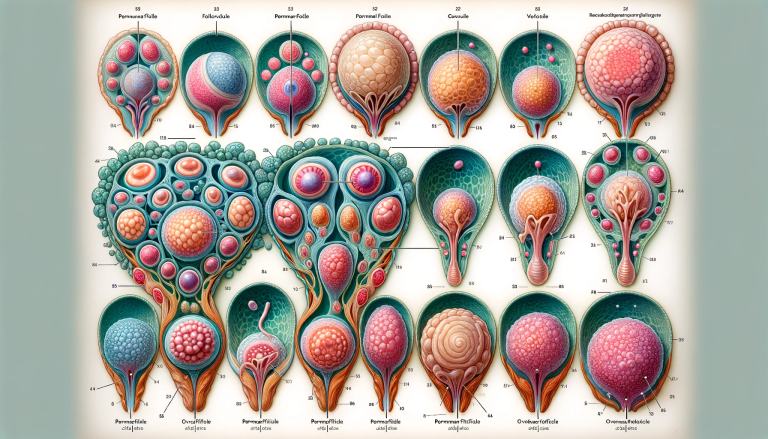
Ovarian follicles, also known as antral follicles, are small 2mm to 8mm, sac-like structures in the ovaries that contain a developing egg. Follicles are the basic functional unit of the female reproductive system and play a key role in fertility. When reproductive hormones surge during a menstrual cycle, one or more follicles will begin to mature and release an egg for potential fertilization.
The prevalent understanding indicates that women are born with about 300,000 to a million eggs. These undergo spontaneous degeneration. At the age of 38 about 25,000 remains in the ovaries. Thereafter, women lose eggs at a faster rate, till eggs are exhausted near the age of menopause at around 50 years old.
During a woman's childbearing years, multiple ovarian follicles will begin to grow each month, with only one maturing enough to release an egg for ovulation. From this point on, these follicles will shrink and die if they go unfertilized. As women age and reach menopause, they experience declines in both their number of remaining follicles and their quality. This is referred to as ovarian reserve or ovarian aging – a decrease in the potential number of eggs left available for fertilization that can make conception more difficult with advanced maternal age.
What is Ovarian Reserve?
Ovarian reserve is a measure of the number and quality of eggs that a woman has. It is an important factor for fertility, as it helps to determine how likely a woman is to conceive either naturally or with assisted reproductive treatment such as IVF.
Measuring ovarian reserve involves performing blood tests to measure hormone levels, as well as transvaginal ultrasound scans to check the overall size, structure and health of the ovaries.
Knowing your ovarian reserve can be beneficial when planning to start a family or for fertility treatment to make informed decisions about conception and childbearing options.
Factors Affecting Ovarian Reserve
There are various factors affecting a woman's ovarian reserve such as:
-The length of time regularly ovulating
-Exposure to toxins (such as radiation or chemotherapy)
-Genetic history
-Health issues including diabetes, obesity, endometriosis, polycystic ovarian syndrome, uterine fibroids
-Age; the time frame during which fertility gradually decreases starting at age 35
Testing Ovarian Reserve
A doctor will normally use blood tests, ultrasound or both to evaluate a woman's fertility.
Blood tests evaluate the hormone levels of a woman such as:
Follicle Stimulating Hormone (FSH) which is a marker for measurement of ovarian reserve because it reflects the function of the ovary and its response to hormones released by the brain’s pituitary gland
Luteinizing Hormone (LH) is also involved with ovarian reserve, but its role is not essential for hormonal testing due to its low accuracy when diagnosing low ovarian reserves.
Anti-Müllerian Hormone (AMH) is a hormone secreted from the primary follicles in the ovaries and serves as one of the most reliable metrics for predicting ovarian reserve., and
Estradiol (E2) can help assess egg quality and it's elevated with conditions like polycystic ovary syndrome (PCOS).
A transvaginal ultrasound exam will measure number and size of antral follicles present in each ovary at any given time. This helps determine the likely number of primary follicles which develop into eggs during each menstrual cycle.
What are the benefits of testing for ovarian reserve?
1. For women: to have some insight into the chances for success of their fertility treatment
2. For their reproductive endocrinologists: to be able to tailor fertility treatments to improve success rates. The low ovarian reserve may require modification of fertility medication or applying other methods to improve response.
3. In fertility preservation: the success of preservation is especially related to egg reserve. In the majority of cases, freezing of eggs and embryos is considered for the preservation of fertility.
4. In women exposed to chemotherapy: exposure to cyclophosphamide and other agents markedly reduces egg reserve. Very young women exposed to less toxic treatments may preserve their future fertility after cancer treatment.
What do My Antral Follicle Levels Mean?
- Less than four antral follicles: This is a very low count. This suggests that your ovaries will have an extremely poor response to ovarian stimulation.
- 4-6 antral follicles: This is a fairly low count.
- 7-10 antral follicles: This is still a fairly low count with the lower chance of ultimate pregnancy success.
- 11-15 antral follicles: This is the lower end of the 'average'. Usually, ovarian stimulation has reasonable results but can be on the low side. Pregnancy success rates are fair but not excellent.
- 16-30 antral follicles: This is a good antral count, which is likely to have an excellent response to ovarian stimulation even with low doses of FSH.
- Over 30 antral follicles: This is a worryingly high count, which might indicate a polycystic ovary.
The ultrasound scan
There are two basic kinds of ultrasound used to evaluate the female pelvic organs - an abdominal ultrasound, which involves passing the scanner over the abdomen, and a vaginal ultrasound, which involves inserting the scanner through the vagina.
Vaginal ultrasounds are normally used for monitoring the follicles because they provide a more accurate picture of the ovaries and follicles than an abdominal scan.
During the ultrasound, a small ultrasound probe will be placed into your vagina and will be moved in different directions to obtain the required images.
Treatments for Low Ovarian Reserve
Women with a low ovarian reserve may have difficulty conceiving due to their decreased egg production. To increase the chances of pregnancy, there are several treatments for women with low ovarian reserve. These may include hormone therapy, medications to encourage ovulation, in-vitro fertilization (IVF), or intracytoplasmic sperm injection (ICSI).
Hormone therapy is used to encourage the production of eggs in a woman with low ovarian reserve. Medications used to stimulate ovulation may include clomiphene citrate or gonadotropins. These medications help release an egg during each menstrual cycle, potentially increasing the chances of successful conception.
IVF is usually used when hormone therapy and drugs fail. During this procedure, eggs are surgically removed from the ovarian follicles and fertilized outside the body with sperm from either a partner or donor. If multiple mature eggs are obtained, they can be frozen for later use if desired by the couple. Intracytoplasmic sperm injection (ICSI) is another type of IVF procedure in which one sperm cell is injected directly into each egg to improve chances of successful fertilization and implantation.
In vitro maturation (IVM) is considered a less invasive option than IVF as it does not require anaesthesia or an injection of hormones to stimulate the ovaries prior to harvesting eggs. The eggs are allowed to mature naturally inside the body before being retrieved for either manual or assisted fertilization procedures such as ICSI, eliminating some risks associated with IVF treatments such as multiples births and ectopic pregnancy.
Good to know
Abnormal value of these or other tests does not automatically indicate that a woman should be prevented from trying using her own eggs. The predictive ability of these tests is modest and not absolute (these tests can make mistakes).
The results of these tests should be carefully interpreted by a reproductive endocrinologist. Generally women should not be denied treatment based on the test result alone. These tests have low ability to predict the occurrence of pregnancy.
Tests for ovarian reserve cannot directly predict the quality of individual eggs or embryos. Age is a better predictor of egg quality.