Polycystic ovary syndrome (PCOS) is a common hormonal disorder that affects women of reproductive age. It is characterized by irregular menstrual cycles, excess androgen levels, and polycystic ovaries (ovaries with many small, fluid-filled cysts). While the exact cause of PCOS is unknown, it is thought to be related to insulin resistance and androgen excess.
Follicular scans, also known as ovarian ultrasounds, are an important diagnostic tool and monitoring method for women with PCOS. This article will provide an overview of PCOS and discuss the role of follicular scans in diagnosis and management.
What is Polycystic Ovary Syndrome (PCOS)?
PCOS is estimated to affect 6-12% of women of reproductive age worldwide, making it one of the most common hormonal disorders. The three key features of PCOS are:
- Irregular periods - Women with PCOS often have oligomenorrhea (cycles longer than 35 days) or amenorrhea (absent periods). This is due to irregular ovulation.
- Hyperandrogenism - Elevated male hormones like testosterone. Signs include excess facial and body hair growth, scalp hair loss, acne, and oily skin.
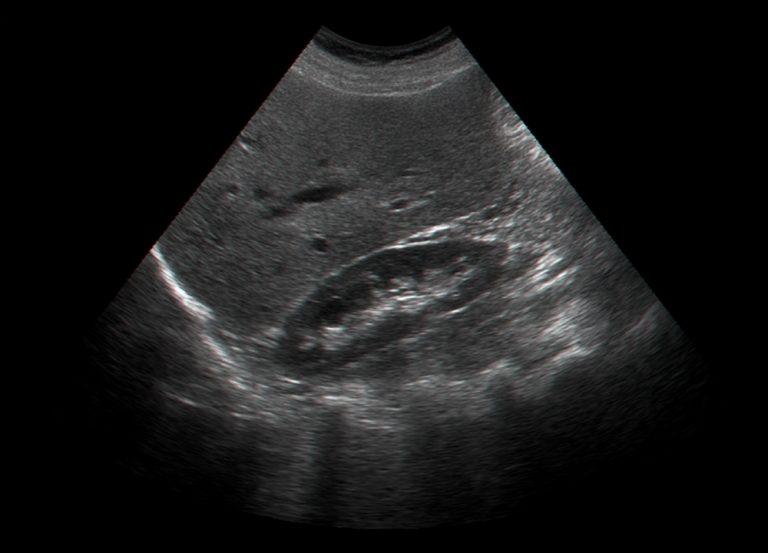
- Polycystic ovarian morphology - Ovaries appear enlarged with many small follicles seen on ultrasound. Typically one ovary is larger than the other.
While these are the classic triad of symptoms, PCOS manifests differently in each woman. Many also struggle with obesity, insulin resistance, infertility, and mental health issues like anxiety and depression.
PCOS is a complex condition with impacts across the lifespan. It is important for symptomatic women to seek diagnosis and treatment, as there are many options available to manage PCOS.
Diagnosing PCOS with Follicular Scans
There is no single test to diagnose PCOS. Doctors will take a full history, perform a physical exam, and run bloodwork to look for elevated androgens, irregular cycles and ovulation, and rule out other possible causes.
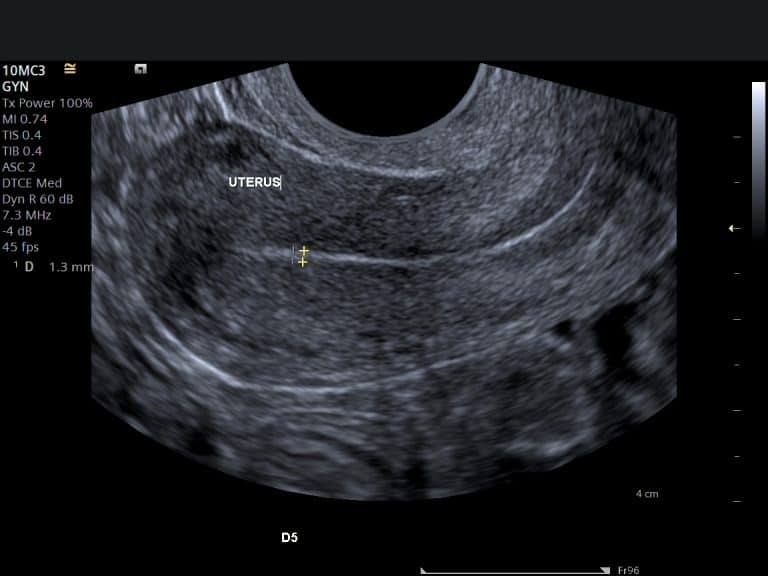
One of the key diagnostic criteria is evidence of polycystic ovaries on ultrasound. This requires a trained technician to perform a transvaginal follicular scan.
What is a follicular scan?
A follicular scan examines the ovaries and developing follicles (fluid-filled sacs that contain the eggs). It allows measurement of ovarian volume and follicle count.
In PCOS, the ovaries are often enlarged and contain many small, cyst-like follicles arranged around the edge of the ovary in a pearl necklace pattern. Typically one ovary is larger than the other.
Follicular scans can confirm polycystic ovarian morphology (PCOM), which is one of the diagnostic criteria for PCOS according to the Rotterdam criteria.
Who should get a follicular scan for PCOS?
Guidelines recommend a follicular scan for women with:
- Irregular menstrual cycles
- Signs of androgen excess like hirsutism, acne, and hair loss
- Obesity
- Infertility
The scan should be done early in the menstrual cycle (cycle days 2-5) when follicles are small and easier to visualize and count.
Timing is important as later in the cycle a dominant follicle may form, obscuring the view of small follicles indicative of PCOS.
Interpreting the results
There are clear cutoff values used to define polycystic ovaries:
- Ovarian volume ≥10 mL (each ovary)
- Follicle number per ovary ≥12
- Follicles measuring 2-9 mm in diameter
However, polycystic ovarian morphology alone does not definitively diagnose PCOS. Only 12-18% of women with polycystic ovaries on ultrasound actually have the endocrine and metabolic features of PCOS.
That's why follicular scans are combined with clinical history, physical exam, and bloodwork to make a comprehensive PCOS diagnosis.
Role of Follicular Scans in Managing PCOS
In addition to diagnosis, ovarian ultrasounds play an important role in ovulation monitoring and treatment for women with PCOS trying to conceive.
Ovulation monitoring
One of the main goals of PCOS treatment is to induce regular ovulation. This can be achieved through lifestyle changes, medication, or a combination approach.
Follicular scans allow doctors to track follicular development and identify when/if ovulation occurs by monitoring:
- Follicle growth and maturation
- Endometrial thickening
- Eventual rupture and collapse of the dominant follicle
This information helps time intercourse or insemination appropriately.
Ovulation prediction kits that measure urine LH levels are often ineffective in PCOS. Follicular scans give much more reliable information for ovulation tracking.
Treatment monitoring
Ovarian ultrasounds are frequently used to monitor response to ovulation induction therapies like:
- Clomiphene citrate - Follicular scans monitor follicle growth and prevent overstimulation.
- Letrozole - Monitoring is recommended to time intercourse and reduce multiple gestations.
- Gonadotropins - Very close monitoring needed due to higher pregnancy rates and ovarian hyperstimulation risk.
Monitoring follicle development and estrogen levels guides medication adjustment to achieve ovulation while avoiding ovarian hyperstimulation syndrome (OHSS).
Scans are also useful for monitoring response to ovarian drilling procedures intended to stimulate ovulation.
Beyond fertility treatment
While ovulation monitoring is their primary role in PCOS management, follicular scans may also help:
- Assess endometrial health prior to embryo transfer in IVF
- Monitor ovarian cysts
- Evaluate ovarian enlargement or masses
So in summary, follicular scans are an important diagnostic and monitoring tool for women with PCOS seeking fertility treatment. They allow precise tracking of follicular development and ovulation to time treatment and interventions appropriately.
What to Expect During a Follicular Scan
Many women feel nervous about having a transvaginal ultrasound. Here's a quick run-through of what to expect:
- Full bladder not needed - For pelvic scans the bladder is filled, but a full bladder interferes with visualizing the ovaries. Come with an empty bladder.
- Transvaginal probe - The ultrasound probe is slender wand-shaped transducer that is inserted in the vagina to get closer to the ovaries. This gives much clearer images than abdominal scanning.
- Relaxation and lube - Breathe deep and try to relax your muscles. The probe is lubricated to ease insertion. Inform your technician if you have pain/discomfort.
- Pressure - You may feel some pressure as the probe is inserted, but it should not be overly painful. Take slow deep breaths and let your provider know if you need a break.
- Viewing the ovaries - The technician will move the probe around to visualize the ovaries and developing follicles. It generally takes 10-15 minutes to get all the measurements.
- Discussion - Your provider will discuss the results with you shortly after the scan and also follow up with final scan reports. Ask questions!
While transvaginal scans may cause some short-term discomfort, the vital information they provide is worthwhile for women with PCOS trying to conceive.
What Else Should I Know About PCOS and Fertility?
Follicular scans are one piece of the fertility puzzle for women with PCOS. Here are some other key points about PCOS and getting pregnant:
- Ovulation is irregular - Lack of ovulation is a major cause of infertility in PCOS. The first goal is kickstarting regular ovulation, which follicular scans can help monitor.
- Lifestyle changes matter - Losing just 5% of your body weight can improve ovulation, hormone balance, and fertility. A healthy diet and exercise regimen should be the foundation.
- Ovulation medications - Clomiphene and letrozole are commonly used to induce ovulation. Gonadotropins may also be used for women who don't respond to pills alone.
- Metformin treatment - The diabetes drug metformin helps improve insulin sensitivity and regulate ovulation. It may be used alone or in combination with ovulation meds.
- Reproductive assistance - Treatments like IUI or IVF may be needed if ovulation induction medications are unsuccessful after 6 months. Seek a reproductive endocrinologist.
- Don't wait - Seek help sooner rather than later if you don't have regular cycles and are trying to conceive. There are many options to explore.
The key is working with a multi-disciplinary team including your gynecologist, reproductive endocrinologist, nutritionist, and mental health provider. Be patient and persistent - it may take some trial and error to find the ideal treatment path for your PCOS.
In Conclusion
Polycystic ovarian morphology seen on ultrasound is one of the diagnostic criteria for PCOS. Follicular scans allow assessment of ovarian volume and follicle number, aiding diagnosis.
Ovarian ultrasounds are also essential for monitoring ovulation and timing intercourse or insemination when trying to conceive with PCOS. They provide crucial data to guide responsive fertility treatment.
While the scans may cause temporary discomfort, the information gained is extremely valuable. When combined with bloodwork and physical exam, follicular scans give your provider important insight to customize an effective PCOS treatment plan.
If you have PCOS and are looking to get pregnant, don't lose hope. Work with a team of experts, leverage tools like follicular scans to time treatment, and be consistent with healthy lifestyle changes. Many women with PCOS do go on to have healthy pregnancies and babies with the right support.