Ultrasound imaging has become an integral part of fertility care and treatment. From initial fertility assessments to monitoring ovulation and uterine health during treatment cycles, ultrasound provides important visual information for reproductive specialists and their patients.
Uses of Ultrasound in Fertility Care
Ultrasound serves several key purposes in fertility care:
- Initial fertility assessments
- Ovarian monitoring
- Uterine evaluations
- Pregnancy monitoring after conception
- Guidance during fertility procedures
Initial Fertility Assessments
An ultrasound is often one of the first tests performed as part of a fertility workup. It allows physicians to visualize the reproductive organs and identify any structural problems or abnormalities.
Some key aspects evaluated during initial ultrasound assessments include:
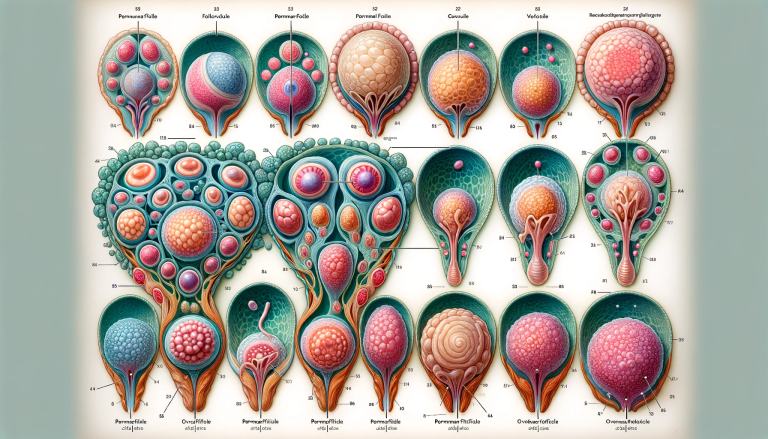
- Ovarian reserve - The number and appearance of follicles provides information about ovarian reserve, or the remaining supply of eggs. A lower number of antral follicles indicates diminished ovarian reserve.
- Uterine structure - The size, shape and contour of the uterus is evaluated. Fibroids, polyps or other uterine abnormalities can be detected.
- Endometrial lining - The thickness and appearance of the endometrium is noted. An irregular or thin lining may indicate health issues.
- Fallopian tubes - Fluid around the tubes may indicate a blockage.
Initial ultrasound assessments create a picture of ovarian function and uterine health to help guide treatment recommendations.
Ovarian Monitoring
Once fertility treatments begin, ultrasound is used to carefully monitor ovarian response and follicle development.
During ovulation induction cycles, ultrasounds are performed every 1-3 days to track follicle growth and identify the dominant follicle(s). Key parameters include:
- Number of follicles
- Size of each follicle
- Appearance and thickness of the follicle lining
This monitoring allows the care team to time intercourse or insemination appropriately. Ultrasound also guides decisions about cycle cancellation if too few or too many follicles develop.
For IVF treatment, ultrasounds play a critical role in monitoring follicular response to fertility medications. Frequent ultrasounds track the cohort of developing follicles and inform decisions about medication dosing. Once lead follicles reach an appropriate size, an ultrasound guides the timing of egg retrieval.
Following egg retrieval, ultrasounds continue to evaluate the ovaries and ensure they are returning to normal size after aggressive follicle growth.
Uterine Evaluations
In addition to monitoring the ovaries, ultrasound evaluations focus on the health of the uterine lining during treatment.
Endometrial appearance is monitored as it thickens and prepares for implantation. An irregular or thin lining can indicate health issues and lead to cycle cancellation.
Ultrasound is also used to further assess and monitor uterine fibroids. Depending on the size and location, fibroids can impact the likelihood of conception and healthy implantation.
Throughout treatment, ultrasound allows providers to ensure the uterus is ready to support embryo implantation and early pregnancy.
Pregnancy Monitoring
Ultrasound continues to provide valuable information after conception occurs.
About two weeks after a positive pregnancy test, ultrasound is used to:
- Confirm pregnancy placement (intrauterine or ectopic)
- Check for a fetal heartbeat
- Measure the gestational sac
- Assess the health and development of the early embryo/fetus
Additional ultrasounds are often performed during the first trimester to monitor growth, check for twins/multiples, and screen for potential issues. Ultrasound allows providers to track the progress of the pregnancy and screen for problems.
Later in pregnancy, ultrasound is used to evaluate fetal growth and position, the placenta, and amniotic fluid levels.
Guidance for Fertility Procedures
In addition to diagnostic imaging, ultrasound technology provides real-time visualization that guides fertility specialists during many hands-on procedures.
Some examples include:
- Follicle aspiration - Ultrasound guides the needle during egg retrieval for IVF. This ensures accurate follicle targeting.
- Embryo transfer - After IVF, ultrasound allows precise positioning of the transfer catheter to optimize embryo placement.
- Intrauterine insemination (IUI) - Ultrasound enables the specialist to visualize the catheter path through the cervix into the uterus.
- Hysteroscopy - Ultrasound may be used alongside the hysteroscope camera to provide additional visualization during uterine evaluation and surgery.
- Endometrial biopsy - During this procedure, ultrasound helps guide proper instrument placement for tissue sampling.
The real-time visual guidance makes many fertility procedures easier, safer, and more effective.
Ultrasound Technology in Fertility Care
There are two main types of ultrasounds used in gynecologic and fertility care:
Transabdominal Ultrasound
In this approach, the ultrasound probe (transducer) is moved over the abdomen to obtain images of the reproductive organs through the abdominal wall. A gel lubricant is applied to enhance contact and image transmission.
Transabdominal ultrasound provides excellent visualization of the uterus and ovaries. One limitation is that a full bladder is needed to give the transducer a wider window for imaging.
This type of ultrasound is commonly used for initial screenings, ovarian monitoring, and pregnancy monitoring. The overall size and position of fibroids and other uterine issues can also be observed.
Transvaginal Ultrasound
With this intimate method, the transducer probe is inserted into the vaginal canal to obtain detailed images of the reproductive structures.
The transducer lies closer to the ovaries and uterine lining, allowing more detailed evaluation. Having the probe inserted vaginally also eliminates the need for a full bladder.
Transvaginal ultrasound provides the most clear, close-up views of the ovaries, follicles, uterine lining, and early gestational sac/embryo. This approach is essential for detailed ovarian monitoring and early pregnancy confirmation.
Many practices start with transabdominal ultrasound and switch to transvaginal for more detailed viewing when needed. Both methods have distinct advantages in fertility care.
Benefits of Ultrasound for Fertility
There are many benefits to using ultrasound for fertility assessment and treatment:
- Non-invasive - No needles, incisions or radiation exposure. There are no known risks with standard diagnostic use.
- Cost-effective - Less expensive than many other imaging modalities. Ultrasound also reduces costs by directing care, avoiding unnecessary procedures, and monitoring treatment safely.
- Convenient - Ultrasounds are performed in the fertility clinic. No separate facility visits are required. Studies are quick, with no major preparation needed.
- Patient comfort - Well-tolerated with minimal, if any, discomfort. Allows patients to be actively involved, unlike sedation-requiring methods.
- Multiple uses - One modality serves many diagnostic and treatment purposes, from initial intake through pregnancy.
- Accuracy - Provides clear, high-resolution images allowing detailed reproductive assessments. Results aid in evidence-based care decisions.
Understanding Ultrasound Results
Ultrasound creates visual data that must be skillfully interpreted by trained professionals. The diagnostic radiologist who performs and reads the study conveys results to the treating fertility specialist.
Key ultrasound findings typically include:
- Number, sizes and appearance of ovarian follicles
- Thickness and echotexture of endometrial lining
- Size, shape and surface of uterus and fallopian tubes
- Presence/appearance of masses (fibroids) or fluid
- Gestational sac parameters and embryo measurements
- Fetal number, heart rate, position and movement
The radiology report communicatestechnical impressions to the physician through ultrasound-specific terminology. Patients review the key findings and their implications for treatment with their fertility doctor.
Asking questions can help patients better understand how ultrasound findings relate to fertility health, treatment options and prognosis. Areas of uncertainty should be discussed.
Risks and Limitations of Fertility Ultrasound
Standard diagnostic ultrasound is considered very safe with minimal risks in trained hands. Limitations include:
- User skill/experience impacts image quality and interpretation accuracy. Results rely on the sonographer’s technique and the radiologist’s diagnostic expertise.
- Image quality reduced by obesity, intestinal gas or abdominal scarring. Difficulty visualizing ovaries and uterus may require transvaginal ultrasound or could limit assessment.
- Does not assess fallopian tube patency. A hysterosalpingogram or laparoscopy is needed to confirm tubal blockage.
- Limited sensitivity detecting some uterine issues like adenomyosis or scar defects within the uterine cavity. MRI may provide additional information.
- Can not confirm ovulation occurred. Serial ultrasounds show follicle development, but hormone testing is needed to confirm ovulation.
- Twin detection in early pregnancy not 100% accurate. A follow-up scan may be needed to confirm initial findings either way.
- Unable to detect all fetal structural anomalies or problems. Additional screening may be recommended.
- User/patient discomfort during transvaginal ultrasound possible but usually minimal.
Overall, ultrasound is a safe, accessible and highly effective fertility assessment and monitoring tool. Understanding the scope and limits of its diagnostic capabilities is important. Additional testing may be warranted depending on scan findings and clinical concerns.
Questions to Ask About Fertility Ultrasound
Undergoing ultrasounds during fertility care often brings up many questions for patients. Asking questions helps you play an active role in treatment decisions.
Some key questions patients may want to ask their fertility specialist include:
- What are the next steps based on my ultrasound results?
- How will the findings impact my treatment plan?
- Do the results indicate any problems or issues to address?
- How many follicles/eggs should be expected? Is this number normal for my age?
- Is my endometrial lining favorable for implantation?
- Do any fibroids or cysts found require treatment or removal?
- Could a transvaginal scan provide a clearer picture?
- How often will ultrasounds be performed to monitor treatment?
- When should I expect to see a gestational sac or fetal heartbeat on ultrasound?
- Do multiple sacs or embryos indicate twins/multiples? How accurate is this early prediction?
- At what point would you recommend additional diagnostic imaging?
Do not hesitate to ask your doctor to explain ultrasound findings, recommendations and next steps. Share any specific concerns or fears you have surrounding ultrasound results and fertility implications.
Your provider can help you understand the role of ultrasound for your particular condition and treatment protocol.
Finding a Reproductive Ultrasound Specialist
If pursuing fertility treatments, you want to find a clinic with radiology staff experienced in gynecologic and reproductive ultrasound. Ask these questions when researching providers:
- How many years has the clinic been performing fertility ultrasounds?
- Are sonographers specially trained in reproductive imaging?
- Will the ultrasounds be performed by an OB-GYN radiologist?
- Are same-day ultrasound appointments available for urgent monitoring?
- Do they use advanced ultrasound technology for optimal images?
- Can ultrasound guidance be provided for egg retrieval, embryo transfer, etc?
Seeking a center of excellence with dedicated fertility radiology specialists can optimize this vital component of your care.
The Takeaway
Ultrasound technology allows fertility specialists to visualize and monitor the ovaries, uterus and developing pregnancy. This critical imaging modality informs treatment planning and decision-making from initial intake through conception.
While extremely beneficial, ultrasound has limitations requiring supplementation at times with other testing. Understanding ultrasound's diagnostic capabilities and asking questions empowers patients to participate in their fertility care. Seeking experienced reproductive imaging specialists helps further enhance this key component of treatment.
References:
Footnotes
Applications of intraoperative ultrasound in gynecological surgery - A. Criniti, P. Lin, 2005.
Monitoring stimulated cycles during in vitro fertilization treatment with ultrasound only – preliminary results - A. Wiser et al., 2012.
Ultrasound control of clomiphene/human chorionic gonadotropin stimulated cycles for oocyte recovery and in vitro fertilization - I. Hoult et al., 1981.
The effect of ultrasound exposure in utero on the development of the fetal mouse testis: adult consequences - K. Carnes et al., 1995.
Role of Pelvic Ultrasound in Girls with Precocious Puberty - L. de Vries, M. Phillip, 2011.
Transvaginal ultrasound-guided embryo transfer improves outcome in patients with previous failed in vitro fertilization cycles - Robert E. Anderson et al., 2002.
The role of ultrasound in ovulation induction: a critical appraisal - M. Seibel et al., 1981.
'Without ultrasound you can't reach the best decision' - A. Åhman et al., 2018.
Ultrasound as a useful imaging modality for tumor detection and staging - C. Mittelstaedt, 1980.