Fertility Ultrasound Scans in London
Trying to conceive, starting fertility treatment, or investigating reproductive symptoms? Fertility ultrasound scans provide detailed, real-time imaging of the reproductive organs to support planning and clinical decision-making for both women and men.
At International Ultrasound Services (IUS London), we offer a focused set of fertility-related ultrasound scans, performed by experienced clinicians, with clear explanation of findings and a written report.
Not sure which scan you need? Use the guide below, or contact our team and we’ll help you choose the most appropriate option based on your goal.
Choose the right fertility scan
If your goal is ovulation timing or cycle monitoring
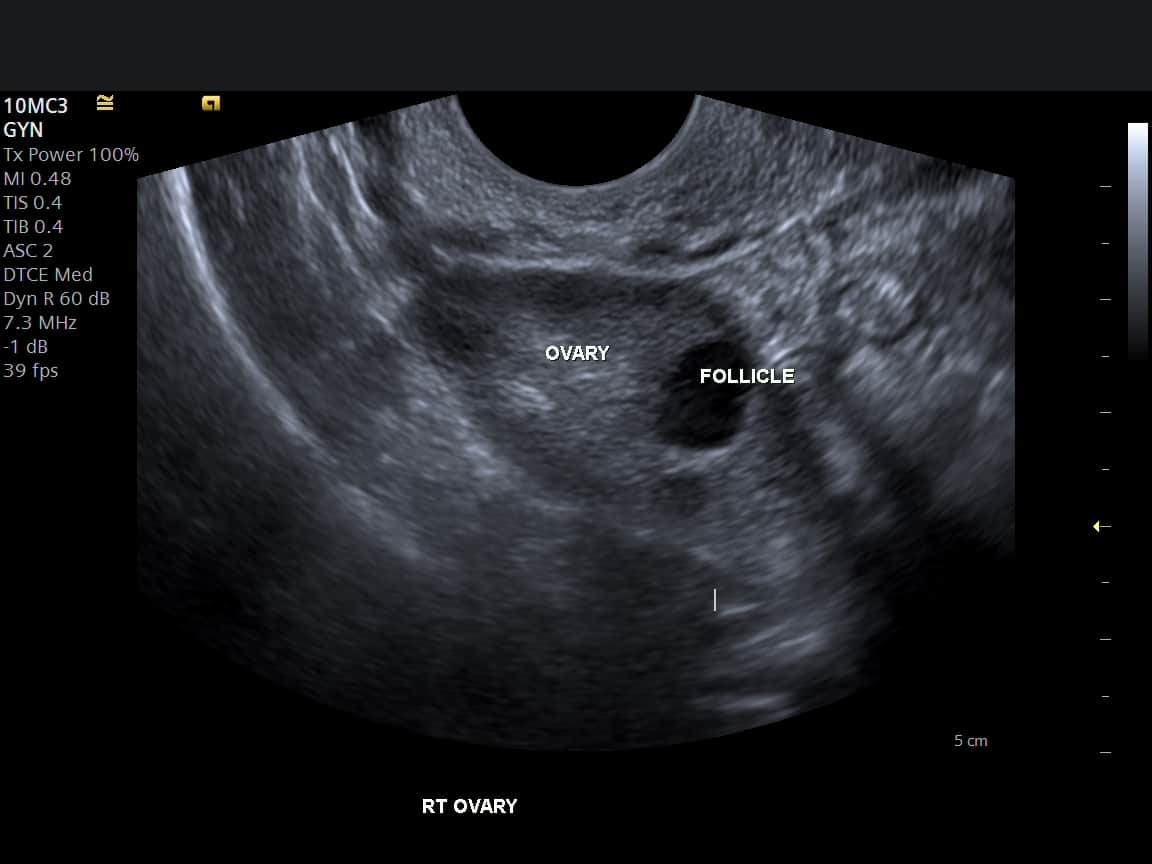
Recommended: Follicle Tracking Scan (Ovulation Monitoring)
Best for understanding follicle growth and identifying the most fertile window.
If your goal is an ovarian reserve estimate
Recommended: AFC Scan (Antral Follicle Count / Ovarian Reserve)
Best for baseline fertility planning and treatment discussions (commonly early cycle).
If your goal is a general uterus and ovaries assessment
Recommended: Pelvic Ultrasound
Useful for fertility planning and/or symptoms such as pelvic pain, irregular bleeding, or known gynaecological history.
If your goal is uterine lining assessment
Recommended: Endometrial Thickness Scan
Focused measurement of the endometrium (uterine lining), often relevant to cycle assessment or treatment monitoring.
View Endometrial Thickness Scan
If your goal is male fertility assessment
Recommended: Testicular (Scrotal) Ultrasound
Useful for evaluating scrotal symptoms and supporting male fertility workups where appropriate.
What is a fertility ultrasound scan?
A fertility ultrasound scan is a diagnostic ultrasound examination used to assess reproductive anatomy and, in some cases, monitor cycle-related changes. Depending on the scan type, ultrasound can help evaluate:
Ovaries: follicles (growth and number), ovarian appearance
Uterus: size, shape and structural features
Endometrium: lining thickness and appearance
Male reproductive anatomy: testes and surrounding scrotal structures
What fertility ultrasound can’t tell you on its own
Ultrasound is one part of fertility assessment. It does not directly measure egg quality, genetics, or all causes of infertility in isolation. Many fertility pathways also involve clinical history, hormone blood tests, and—where relevant—semen analysis or additional investigations arranged by your clinician.
Fertility scans we offer
Choose a scan based on your goal (ovulation monitoring, ovarian reserve, uterine lining assessment, pelvic evaluation, or male fertility assessment). Each service links to full details and online booking.
Ovulation monitoring
Follicle Tracking Scan
Best for: timing ovulation and monitoring follicle development across your cycle.
- Tracks follicle growth over time (often across more than one scan)
- May include endometrial (uterine lining) assessment where relevant
- Useful for natural conception planning or fertility clinic monitoring

Ovarian reserve
AFC Scan (Antral Follicle Count)
Best for: a baseline ovarian reserve estimate to support fertility planning.
- Counts small resting follicles in each ovary (where visualised)
- Commonly booked early in the cycle (often days 2–5)
- Helpful for IVF planning, fertility preservation, and baseline assessment

Uterine lining
Endometrial Thickness Scan
Best for: measuring the endometrium (uterine lining) in the context of your cycle or treatment.
- Provides a clear endometrial thickness measurement
- Timing depends on your clinical question or fertility clinic protocol
- Report can be shared with your fertility clinic on request
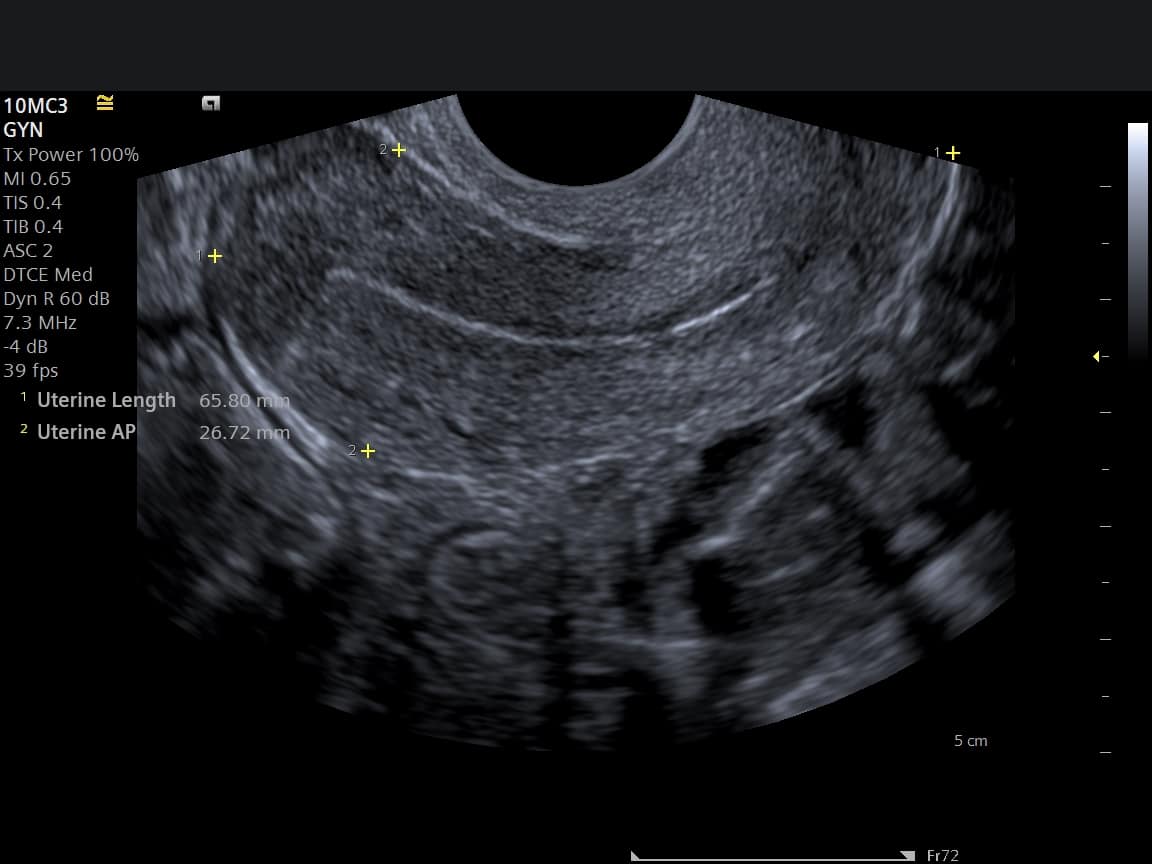
Uterus & ovaries
Pelvic Ultrasound
Best for: a broader assessment of the uterus and ovaries for fertility planning or symptoms.
- Assesses uterus and ovaries as visualised on ultrasound
- May be transabdominal and/or transvaginal (with consent)
- Useful alongside fertility monitoring or symptom investigation

Male fertility
Testicular (Scrotal) Ultrasound
Best for: evaluating the testes and scrotal structures for symptoms and fertility-related questions.
- Assesses testes and surrounding scrotal structures
- No cycle timing required
- Written report suitable for onward clinical discussion
If you are already under a fertility clinic, bring your protocol (medications and target scan days) so the scan answers the correct clinical question.
Compare fertility scans
Fertility ultrasound scans answer different questions. Use the comparisons below to choose the right scan for your goal, then view full details and booking.
Follicle Tracking vs AFC: what’s the difference?
| Dimension | Follicle Tracking Scan | AFC Scan (Antral Follicle Count) |
|---|---|---|
| Primary question | “When am I likely to ovulate?” / “How is my cycle progressing?” | “What is my ovarian reserve estimate?” |
| Timing | Often performed at multiple points across a cycle (frequency depends on goals and findings). | Commonly booked early cycle (often days 2–5), depending on clinical context. |
| Key measurements | Follicle size and growth trend; uterine lining assessment where relevant. | Count of small antral follicles in each ovary (where visualised). |
| Best for | Ovulation timing support; natural conception planning; monitoring in IUI/IVF pathways where required. | Baseline planning for IVF, fertility preservation discussions, and broader fertility assessment. |
| Output | Trend-based monitoring information (often across more than one scan). | Snapshot baseline measurement for onward clinical interpretation. |
If you want ovulation timing
- Choose Follicle Tracking if you want cycle monitoring.
- Useful if you have a target window for timed intercourse, IUI, or clinic monitoring.
If you want ovarian reserve information
- Choose AFC if you want a baseline ovarian reserve estimate.
- Often scheduled early cycle; bring any fertility clinic protocol if relevant.
If you are unsure, contact the clinic and we will guide you to the most appropriate scan based on your goal and timing.
Transvaginal vs Transabdominal pelvic ultrasound (what to expect)
Pelvic ultrasound can be performed transabdominally (probe on the abdomen) and/or transvaginally (internal probe). The approach depends on the clinical question, your circumstances, and your preference.
| Attribute | Transvaginal pelvic ultrasound | Transabdominal pelvic ultrasound |
|---|---|---|
| How it’s performed | Internal probe placed in the vagina to obtain closer views of the uterus and ovaries. | Probe is placed on the lower abdomen to visualise the pelvic organs through the abdominal wall. |
| Detail level | Often provides higher-detail views of uterus, endometrium and ovaries for certain fertility questions. | Provides a broad overview; detail may be limited depending on anatomy, bowel gas, or bladder filling. |
| Preparation | Typically more comfortable with an empty bladder (follow your booking instructions). | Often requires a comfortably full bladder to act as an acoustic window (follow your booking instructions). |
| Typical use cases | Follicle tracking, endometrial lining assessment, detailed pelvic evaluation when clinically appropriate. | Initial overview, situations where transvaginal scan is not suitable, and complementary views. |
| Comfort | May cause mild pressure; should not be painful. Communicate any discomfort immediately. | Usually minimal discomfort; you may feel gentle pressure on the lower abdomen. |
What to bring
- Cycle dates (last period start date) and typical cycle length
- Your fertility clinic protocol/medication schedule (if applicable)
- Key symptoms and relevant medical/surgical history
After the scan
- Findings explained clearly on the day
- Written report with relevant measurements and observations
- Option to share the report with your fertility clinic on request
What happens at your appointment?
Your appointment is structured to answer your clinical question clearly and efficiently, whether you are planning a pregnancy, monitoring a cycle, or investigating symptoms.
Step-by-step
- Confirm your goal and timing
We confirm your cycle dates (where relevant), symptoms, and the question you want the scan to answer. If you have a fertility clinic protocol, please bring it or share it in advance. - The scan (approach explained)
We explain the scan approach (transabdominal, transvaginal, or scrotal, depending on the service). Consent is obtained before any internal scan approach. - Clear explanation of findings
We talk through what is seen on the day in practical terms, including relevant measurements for your scan type. - Written report
You receive a written report documenting findings and key measurements. If requested, we can share the report with your fertility clinic (please provide contact details).
Consent, privacy and comfort
You will always be asked for consent before a transvaginal scan. You can decline an internal scan approach, and we will explain any limitations this may create for the clinical question.
What to bring
If available, please bring:
- Your cycle dates (first day of your last period) and typical cycle length
- Your fertility clinic monitoring protocol or medication schedule (if applicable)
- Relevant symptoms and key medical/surgical history
Prices
Prices vary by scan type and (where relevant) whether monitoring involves more than one visit. For the most accurate pricing and inclusions, please use the links below.
Follicle Tracking Scan
Cycle monitoring for ovulation timing and follicle growth trends.
AFC Scan (Antral Follicle Count)
Baseline ovarian reserve estimate (commonly early cycle).
Endometrial Thickness Scan
Uterine lining measurement in the context of your cycle or treatment.
Pelvic Ultrasound
Uterus and ovaries assessment for fertility planning or symptoms.
Testicular (Scrotal) Ultrasound
Male fertility and scrotal assessment aligned to symptoms/indication.
Important notes
Fertility ultrasound is a valuable diagnostic tool, but findings must be interpreted in context. If you are under a fertility clinic, your clinician should integrate ultrasound results with your history, any blood tests, semen analysis (where relevant), and your treatment plan.
What ultrasound can and can’t do
- Ultrasound can assess reproductive anatomy and support cycle monitoring (depending on scan type).
- Ultrasound does not directly measure egg quality, genetics, or all causes of infertility on its own.
- Some findings require follow-up with your GP, fertility clinic, or onward investigation.
When to seek urgent medical assessment
- Severe pelvic pain, heavy bleeding, or fever.
- Acute scrotal pain/swelling (particularly sudden onset).
- Any symptoms that feel rapidly worsening or concerning.
Fertility scan FAQs
Answers to common questions about timing, comfort, results, and sharing reports with your fertility clinic.
Do I need a referral?
When in my cycle should I book?
How many follicle tracking scans will I need?
Is transvaginal ultrasound painful?
Can I choose transabdominal only?
What will I receive after the scan?
Can you send my report to my fertility clinic?
Can ultrasound confirm ovulation?
Can ultrasound diagnose the cause of infertility?
What should I bring to my appointment?
If you have urgent symptoms (severe pain, heavy bleeding, fever, or acute scrotal pain/swelling), seek urgent medical assessment.
Why choose IUS London for fertility ultrasound?
Choosing the right provider matters—particularly when timing is important. We focus on high-quality diagnostic imaging, clear communication, and practical reporting for onward care.
Experienced clinicians and robust standards
- Fertility-relevant ultrasound performed by experienced clinicians.
- Clear governance and professional standards aligned to diagnostic practice.
- Respectful care, with consent-led scanning and attention to comfort.
Clear results and clinic-ready reports
- Findings explained on the day in plain language.
- Written report with key measurements relevant to the scan type.
- Option to share your report with your fertility clinic on request.
Convenient London location
- Easy access for local patients and those travelling into London.
- Suitable for time-sensitive monitoring within a cycle.
- Discrete, professional clinic environment.
Designed for fertility decision-making
- Scan options mapped to common fertility questions (timing, ovarian reserve, lining assessment).
- Supports both women’s and men’s fertility pathways.
- Practical guidance on timing and preparation to reduce friction.

Book a fertility scan
If you know which scan you need, you can book online. If you are unsure, contact the clinic and we will guide you to the most appropriate option based on your goal and timing.



