A patient-friendly guide to understanding follicle size, growth, and uterine lining measurements
Key takeaways (read this first)
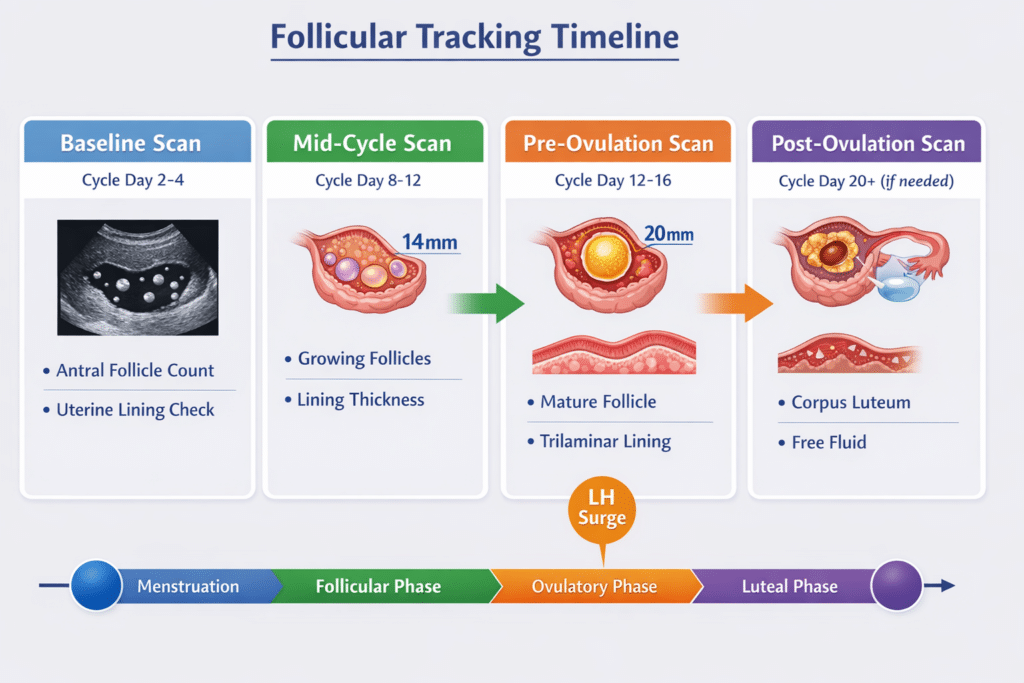
Follicular tracking (also called follicle monitoring or folliculometry) is a series of pelvic ultrasounds used to monitor how your ovarian follicles and uterine lining change across your cycle.
In a natural (unstimulated) cycle, dominant follicles commonly grow about 1.0–1.4 mm/day and may reach a mean diameter of ~20–24 mm around ovulation.
In stimulated cycles, follicles may grow faster (about ~1.7–2.0 mm/day in some protocols).
Endometrial thickness is only one marker of readiness; in assisted reproduction literature, <7 mm is often described as “thin” (with some variation in thresholds), and pattern/appearance can also matter.
A transvaginal ultrasound is widely considered safe, with no radiation and no known side effects for most patients
Why follicular tracking scans can feel confusing
If you are trying to conceive—naturally or with fertility support—each scan can feel like a “pass/fail” moment. I see that anxiety every week.
Our aim at International Ultrasound Services is to translate the measurements on your report into plain English, while being clinically accurate and realistic: ultrasound trends are very informative, but they are only one part of the picture.
What is a follicular tracking scan?
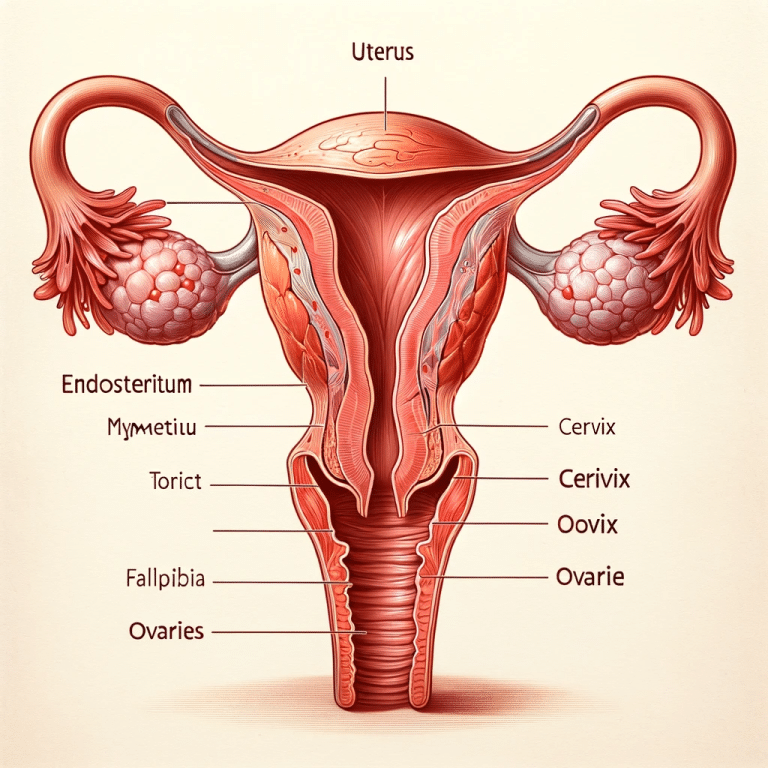
A follicular tracking scan is a pelvic ultrasound (usually transvaginal) performed on one or more days in your cycle to monitor:
Your ovarian follicles (small fluid-filled structures that may contain an egg/oocyte), and
Your endometrium (the uterine lining), which thickens and changes appearance through the cycle.
Clinics use follicular tracking to:
estimate where you are in your cycle,
help time intercourse, insemination (IUI), egg collection (IVF), or a trigger injection,
monitor response to ovulation induction/stimulation medicines,
reduce risks in stimulated cycles (for example, too many developing follicles).
What We measure and report (the “anatomy” of your results)
When I interpret a follicular monitoring scan, I focus on consistent, repeatable parameters:
1) Ovaries: follicle number and follicle size (in millimetres)
Right ovary: sizes of measurable follicles (often those ≥10 mm are tracked closely in treatment cycles), plus any cysts
Left ovary: same
Dominant follicle: the follicle that is clearly leading in size and growth
2) Uterus and endometrium: thickness and appearance
Endometrial thickness is measured in mm on a midline (sagittal) view, using transvaginal ultrasound as the standard approach in most monitoring pathways.
Many reports also describe the pattern (for example, a “trilaminar/triple-line” appearance), particularly around the peri-ovulatory phase.
3) Additional findings that can change the interpretation
Corpus luteum (a post-ovulation structure)
Free fluid in the pelvis (can be seen around ovulation)
Any uterine findings that may matter (fibroids, polyps, adenomyosis features—if visible)
Understanding follicle size and growth
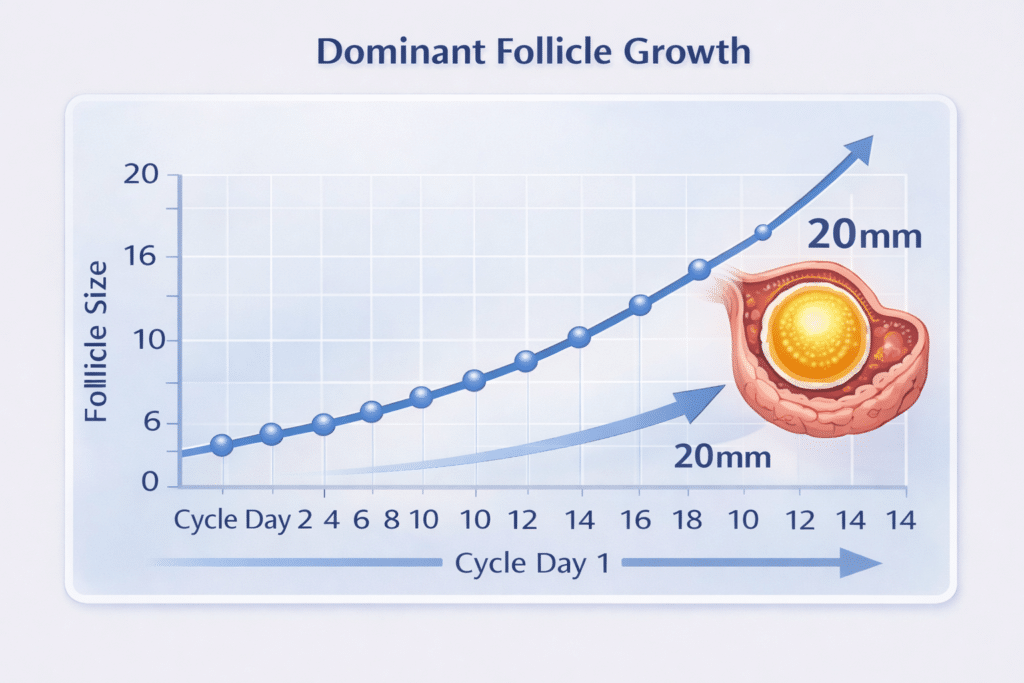
Follicles are dynamic—trends matter more than a single number
One scan is a snapshot. Two or three scans establish a trajectory:
Is a follicle growing steadily?
Is there a clear dominant follicle?
Is growth slower than expected, rapid, or plateauing?
Typical growth rates (natural vs stimulated cycles)
In a natural, unstimulated cycle, dominant follicles are often seen forming around mid-follicular phase and may grow at about 1.0–1.4 mm/day until they reach a mean diameter of ~20–24 mm at the time of ovulation.
In stimulated cycles (e.g., gonadotropin stimulation), follicles may grow faster—reported averages of ~1.7–2.0 mm/day are described in some clinical summaries.
Important: these are population averages. Your protocol, baseline ovarian response, and hormone results can shift the “expected” numbers.
What does “mature follicle” mean?
“Mature” in monitoring usually means “likely approaching ovulation or suitable timing for trigger/egg maturation,” depending on context.
In stimulated cycles, one clinical summary notes that oocyte recovery rates were highest when follicle diameter was ~18–20 mm, and lower when follicles were very small or larger than about the mid-20s.
That does not mean:
ovulation cannot happen outside that range, or
a single follicle measurement guarantees egg quality or outcome.
Interpreting follicle number
Baseline scans and antral follicles (AFC)
A baseline (often cycle day 2–5) scan may describe antral follicle count (AFC)—small follicles visible early in the cycle. AFC is used as one marker of ovarian reserve/response potential, but it is not a fertility verdict on its own.
Why multiple follicles can be good—or risky
In natural cycles, it is common to see one follicle become dominant while others stop growing.
In stimulated cycles, recruiting multiple follicles may be intentional (e.g., IVF), but it can increase the risk of:
multiple pregnancy (in non-IVF pathways), and/or
ovarian hyperstimulation risk (depending on drugs and response).
If I see many growing follicles, I flag it clearly in the report so your prescribing clinic can make safe decisions.
Understanding your endometrial lining results
What endometrial thickness means (and what it doesn’t)
Endometrial thickness is measured by transvaginal ultrasound as the maximal distance between the endometrial interfaces on the midline view.
In assisted reproduction literature:
<7 mm is commonly described as “thin” (though studies use different cut-offs, and pregnancies can still occur below this in some cases).
Pattern can matter too; one review notes that implantation may not be compromised when thickness is ≥6 mm with a trilaminar pattern in some contexts.
Why your lining may look “behind” your follicles
Your lining is hormone-responsive. Common reasons it may appear thinner on a given day include:
later ovulation than expected,
lower oestrogen exposure in that phase,
medication effects (protocol-specific),
individual uterine physiology.
This is exactly why I encourage patients not to over-interpret one measurement in isolation.
Putting it together: how clinicians usually use your scan report
Your fertility clinician typically integrates:
endometrial thickness/pattern (ultrasound),
timing markers (LH surge tests, symptoms),
and sometimes blood tests (oestradiol, LH, progesterone).
In practical terms, your scan helps answer:
Are we approaching ovulation / egg maturation?
Is the uterine lining developing appropriately for this stage?
Is the ovarian response safe (especially in stimulated cycles)?
Common result patterns and what they may lead to (examples)
Below are patterns I frequently see, with typical “next-step” considerations. These are general examples—your clinic’s protocol is the authority.
1) One leading follicle with steady growth
What it often suggests: a natural-cycle pattern or an appropriate response to mild induction.
What usually happens next: your clinic may time intercourse/IUI or plan a trigger based on size trend and hormones.
2) Several follicles growing (stimulated cycles)
What it often suggests: medication-driven recruitment (expected in many IVF/egg freezing cycles).
What usually happens next: the clinic monitors closely to balance success with safety (and may adjust dosage).
3) Follicle growth slower than expected
What it may suggest: delayed follicular development, protocol effect, or individual response variation.
What usually happens next: continued monitoring; possible medication/timing changes (clinic-led).
4) A cyst is noted
What it may suggest: often benign (e.g., functional cyst), but the interpretation depends on appearance and timing.
What usually happens next: sometimes a follow-up scan, sometimes no action—this is context dependent.
5) Lining appears thin for the stage
What it may suggest: simply earlier stage than assumed, or hormone-related variation.
What usually happens next: additional monitoring and correlation with hormones; management is clinic-specific. In ART contexts, “thin” is often discussed around the <7 mm range, but thresholds vary.

What ultrasound cannot tell you (and I make this clear in my consultations)
It cannot directly measure egg quality.
It cannot guarantee the exact moment of ovulation (it estimates likelihood based on size and changes).
It does not replace blood tests where those are clinically indicated.
Is transvaginal follicular tracking safe?
Yes. Ultrasound uses sound waves (not radiation). The NHS notes ultrasound scans do not use radiation, and the sound waves are considered safe. nhs.uk
A transvaginal ultrasound is widely described by UK hospital guidance as a very safe procedure with no side effects. Guy's and St Thomas' NHS Trust
Patient information from the British Medical Ultrasound Society (BMUS) also describes the probe being covered and inserted gently, and that it is usually painless. BMUS
When to seek urgent help
If you are on stimulation medication, do not ignore:
severe abdominal/pelvic pain,
rapid abdominal swelling/bloating,
shortness of breath,
persistent vomiting,
fainting or feeling acutely unwell.
If you are not on stimulation medication, seek urgent review for severe pain, heavy bleeding, fever, or sudden worsening symptoms.
How We structure your report at International Ultrasound Services
When patients come to us for monitoring (including for overseas and UK fertility clinics), I aim to make the report “clinic-ready”:
follicle measurements clearly listed by ovary,
dominant follicle highlighted,
endometrial thickness (and pattern if relevant),
notable findings (cysts, corpus luteum, free fluid),
and a concise, neutral interpretation that supports your clinician’s next decision.
If you are having serial scans, I strongly recommend attending at similar cycle days and, where possible, using consistent timing so trends are easier to interpret.
FAQs
What follicle size means I will ovulate?
Follicle size helps estimate proximity to ovulation, but it is not a guarantee. In natural cycles, a clinical summary describes follicles reaching a mean 20–24 mm at ovulation, with average growth of ~1.0–1.4 mm/day.
How fast should follicles grow?
Growth varies. One clinical summary describes ~1.0–1.4 mm/day in natural cycles and ~1.7–2.0 mm/day in gonadotropin-stimulated cycles.
What is a “dominant follicle”?
It is the follicle that becomes the main developing follicle in that cycle, usually growing larger while others plateau.
What does endometrial thickness mean on my scan?
It is a measurement (in mm) of your uterine lining on ultrasound. In ART literature, <7 mm is often described as thin, but outcomes depend on multiple factors and thresholds vary between studies.
What does “trilaminar” mean?
It describes a “triple-line” appearance that may be seen around the peri-ovulatory period. It is one descriptor of endometrial pattern; it is not a guarantee of implantation or pregnancy.
Is transvaginal scanning painful?
Most patients describe it as uncomfortable rather than painful. UK guidance describes it as similar to an internal examination and generally not painful.
References
Kondagari L, et al. Sonography Gynecology Infertility Assessment, Protocols, and Interpretation (StatPearls). NCBI Bookshelf. 2023. NCBI
Mahajan N. The endometrium in assisted reproductive technology: How thin is thin? J Hum Reprod Sci. 2016. PMC
Guy’s and St Thomas’ NHS Foundation Trust. Transvaginal ultrasound scan – overview (published March 2024; review March 2027). Guy's and St Thomas' NHS Trust
British Medical Ultrasound Society (BMUS). Transvaginal Ultrasound Scan (TVUS) – Patient Information Leaflet. BMUS
NHS. Ultrasound scan (updated 25 Feb 2025).