Nipple discharge can be alarming, particularly when it appears unexpectedly or is blood-stained. In my clinical practice, the most helpful first step is to classify the discharge pattern—because the pattern strongly influences both the likely cause and whether imaging is recommended as part of a diagnostic pathway.
Many causes of nipple discharge are benign, but it should still be checked because a minority of cases require targeted imaging and specialist assessment.
Key takeaways
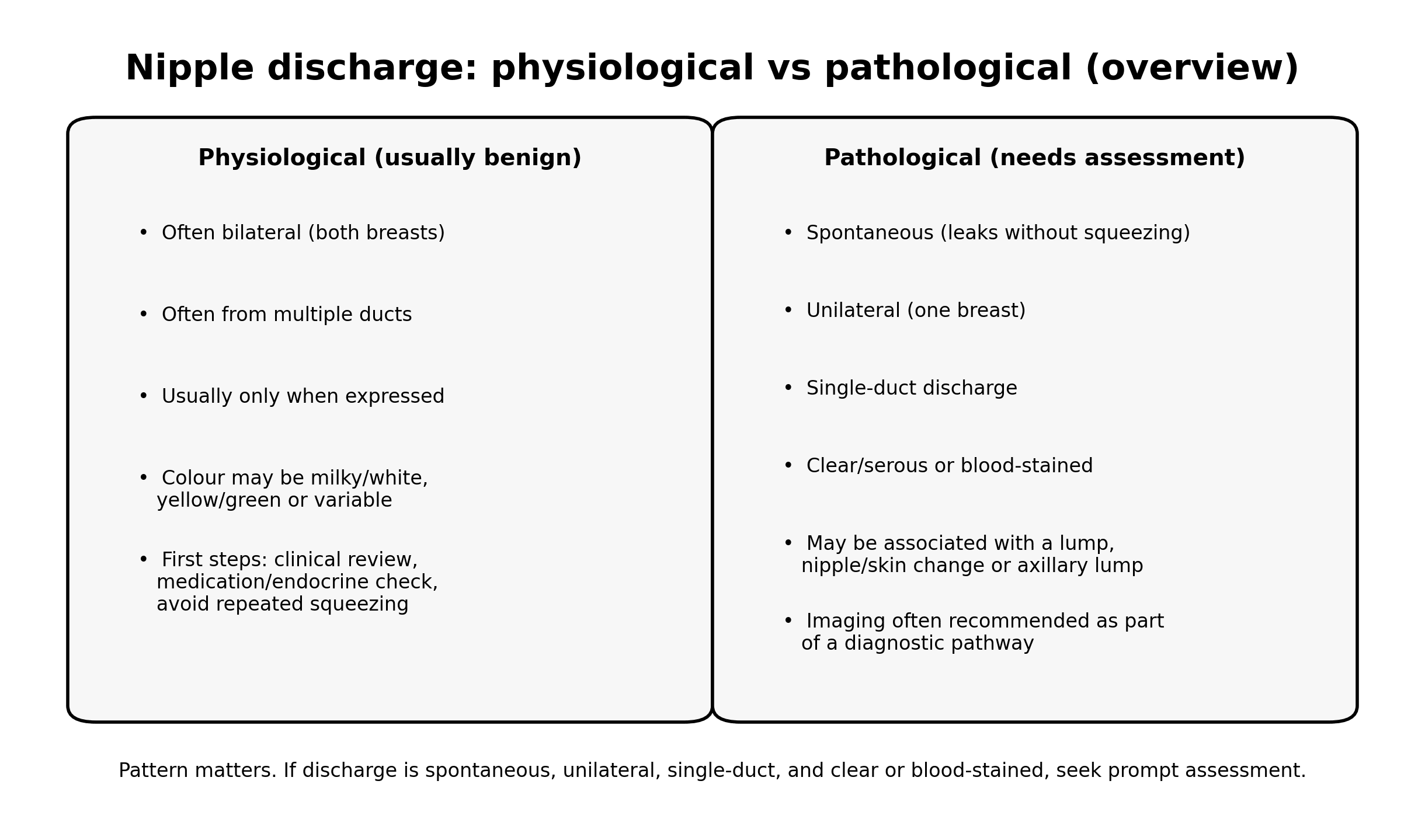
- Discharge is broadly grouped into physiological (often benign) and pathological (more concerning pattern, imaging recommended).
- Spontaneous, unilateral, single-duct, clear/serous or blood-stained discharge is the pattern most likely to trigger imaging in diagnostic pathways.
- In UK pathways, spontaneous unilateral bloody discharge is treated as an urgent assessment feature.
- When imaging is recommended, it commonly includes targeted ultrasound (retroareolar ducts) and mammography depending on age and clinical context; MRI may be used if concern persists despite negative initial imaging.
First: what do we mean by “nipple discharge”?
Nipple discharge means fluid coming from the nipple. It may occur spontaneously (leaks without you touching the breast) or only when expressed (appears when you squeeze the nipple). It can be clear, milky/white, yellow/green, brown, or blood-stained.
Patterns matter: physiological vs pathological discharge
Physiological discharge (usually lower concern)
This pattern is more likely when discharge is:
- from both breasts
- from multiple ducts
- only appears when expressed (not spontaneous)
- milky/white, yellow/green, or variable colours
In these scenarios, imaging is often not the first step. I usually focus on triggers (including avoiding repeated nipple squeezing), review of medications, and endocrine considerations where appropriate.
Pathological discharge (imaging is commonly recommended)
This pattern is more concerning when discharge is:
- spontaneous
- unilateral (one breast)
- from a single duct
- clear/serous or blood-stained
- associated with a lump, skin/nipple change, or enlarged nodes

What nipple discharge usually means: common causes by pattern
Milky discharge (galactorrhoea) when not breastfeeding
Common contributors include:
- hormonal causes (for example raised prolactin)
- medication effects (some antidepressants/antipsychotics, among others)
- thyroid-related issues
- pregnancy (always consider a pregnancy test where relevant)
If discharge is bilateral/milky and otherwise typical of galactorrhoea, the pathway is often clinical assessment plus blood tests, rather than breast imaging as the first step.
Green/yellow/brown discharge
This is often linked to benign duct changes such as duct ectasia (widened ducts with inflammation/debris) and may be intermittent.
Clear/serous or blood-stained discharge (especially single-duct, unilateral, spontaneous)
The most common causes of pathologic discharge are usually benign—particularly intraductal papilloma and duct ectasia. However, significant pathology must be excluded in an appropriate diagnostic pathway, especially when the discharge is blood-stained.
When to seek urgent assessment
Please seek prompt clinical assessment if you have nipple discharge with any of the following:
- Blood-stained discharge that is spontaneous and unilateral
- A new breast lump or focal thickening
- New nipple inversion/distortion, eczema-like nipple change not settling, or skin dimpling
- A new lump in the armpit
- Signs of infection: redness, heat, swelling, fever / feeling unwell
Even if your symptoms do not match the red flags above, it is still sensible to arrange clinical review so the discharge pattern is documented properly.
How I assess nipple discharge clinically (before imaging)
1) Key history questions
- Is it spontaneous or only when expressed?
- One breast or both?
- Single duct or multiple ducts?
- What colour is it (clear/serous, milky, green/yellow, brown, bloody)?
- How long has it been happening? Is it changing?
- Any associated lump, pain, skin change, fever, recent pregnancy/breastfeeding?
- Medication review and endocrine symptoms (where relevant)
2) Focused examination
- Breast and nipple inspection (skin/nipple changes)
- Palpation of breast and axilla
- If discharge is present, I document whether it appears to come from one duct or multiple ducts—this detail often determines the next step in the pathway.
When imaging is recommended in the diagnostic pathway
Imaging is most often recommended when the discharge pattern is pathological—particularly when it is spontaneous, unilateral, single-duct, and clear/serous or blood-stained—or when there is an associated lump or nipple/skin change.

Typical imaging components (selected based on age and clinical concern)
- Targeted breast ultrasound (often focused behind the nipple/areola and any symptomatic area), including axillary assessment when indicated.
- Mammography (more commonly included in women aged 40 and over, or where there is specific clinical concern).
- Breast MRI (a problem-solving tool in selected cases, particularly when discharge remains suspicious but initial imaging is negative).
What imaging can (and cannot) do for nipple discharge
Breast ultrasound
Ultrasound is particularly useful for:
- targeted evaluation behind the nipple (retroareolar region)
- identifying duct dilatation, focal intraduct lesions, cysts, and associated masses
- guiding biopsy if a suspicious abnormality is found

Mammography (and tomosynthesis where used)
Mammography helps evaluate:
- calcifications and architectural distortion (which may not be well seen on ultrasound)
- broader breast assessment where age and clinical concern justify it
Breast MRI
MRI can be considered when the discharge remains clinically suspicious and ultrasound/mammography do not identify a cause. It can help detect occult lesions and guide next steps in selected pathways.
What happens after imaging?
The next step depends on your results and symptoms:
- Benign cause found (for example a papilloma/duct ectasia pattern): management may involve surveillance, symptom control, or referral to a breast surgical team depending on findings and local pathways.
- Indeterminate or suspicious finding: biopsy is usually recommended to complete the diagnostic pathway.
- Imaging normal but discharge remains pathologic: further assessment may include MRI and/or specialist referral, particularly for persistent single-duct blood-stained discharge.
A practical “self-check” before you book
If you are unsure how to describe your discharge, note the following:
- Is it spontaneous?
- Is it one-sided?
- Does it look like it comes from one duct?
- Is it clear/serous or blood-stained?
If the answer is “yes” to these, imaging is more likely to be recommended as part of a diagnostic work-up.
FAQs
Is nipple discharge usually cancer?
No—most nipple discharge is benign. The reason we take certain patterns seriously is that spontaneous, unilateral, single-duct, clear/serous or blood-stained discharge needs assessment and often imaging to exclude significant pathology.
What colour discharge is most concerning?
Colour alone is not enough, but blood-stained discharge—particularly if spontaneous, unilateral, and from a single duct—warrants prompt assessment.
If discharge only happens when I squeeze, should I stop checking?
In many physiological cases, repeated nipple expression can perpetuate discharge. I generally advise avoiding frequent squeezing and arranging clinical review so the pattern is assessed properly.
What imaging will I need?
Imaging is guided by symptoms and age. For concerning discharge patterns, the pathway commonly includes targeted ultrasound and may include mammography; MRI is considered in selected cases if concern persists despite negative initial imaging.
Does nipple discharge in men matter?
Yes. Nipple discharge in men is uncommon and warrants assessment and imaging as part of an appropriate diagnostic pathway.
Booking note (IUS London)
If you have a concerning discharge pattern (spontaneous, unilateral, single-duct, clear/serous or blood-stained) or any red-flag symptom, I recommend prompt clinical assessment. If your pathway supports direct access imaging, you can book appropriate breast imaging at IUS London.
Next step: Contact IUS London to book
Content Information
We review all clinical content annually to ensure accuracy. If you notice any outdated information, please contact us at info@iuslondon.co.uk.
About the Author:

Dr. Mohammad Jalaleddin (GMC number: 7729988) is an internationally-trained physician who earned his medical degree from Tishreen University in Syria in 2005. He completed his specialization in diagnostic radiology in 2009, followed by a Master's degree in 2011, which focused on the radiological alterations of bone grafts. Dr. Jalaleddin has worked as a radiologist in various hospitals and clinics, developing significant expertise in ultrasound and MRI scans. He has extensive experience in performing a wide range of ultrasound examinations, including breast, abdominal, pelvic, and vascular studies. In 2017, he moved to the UK and completed the requalification process with the General Medical Council (GMC). Since March 2021, he has been a part of the Imperial College Healthcare NHS Trust. Dr. Jalaleddin is a member of the General Medical Council (GMC) and the British Medical Ultrasound Society (BMUS).



