Being told you have “dense breasts” can feel worrying, especially if you are already anxious about breast cancer. In my work in diagnostic imaging, I explain breast density in simple terms: density is a mammogram description of how much fibroglandular tissue you have compared with fat. It is common, it is not something you can feel, and it does not mean something is “wrong”.
What density does change is how clearly a mammogram can “see” through the breast tissue, which is why mammography and ultrasound can play different roles depending on the clinical context.
Key takeaways
- Breast density is a mammography finding, not a symptom.
- Dense tissue can make mammograms harder to interpret because dense tissue and many cancers can both look white (the “masking effect”).
- Mammography remains essential for screening and for detecting calcifications.
- Ultrasound is typically a targeted, symptom-led test and can be a helpful adjunct in dense breasts in the right scenario.
- In selected higher-risk pathways, MRI may be considered (case-by-case).
What does “breast density” mean?
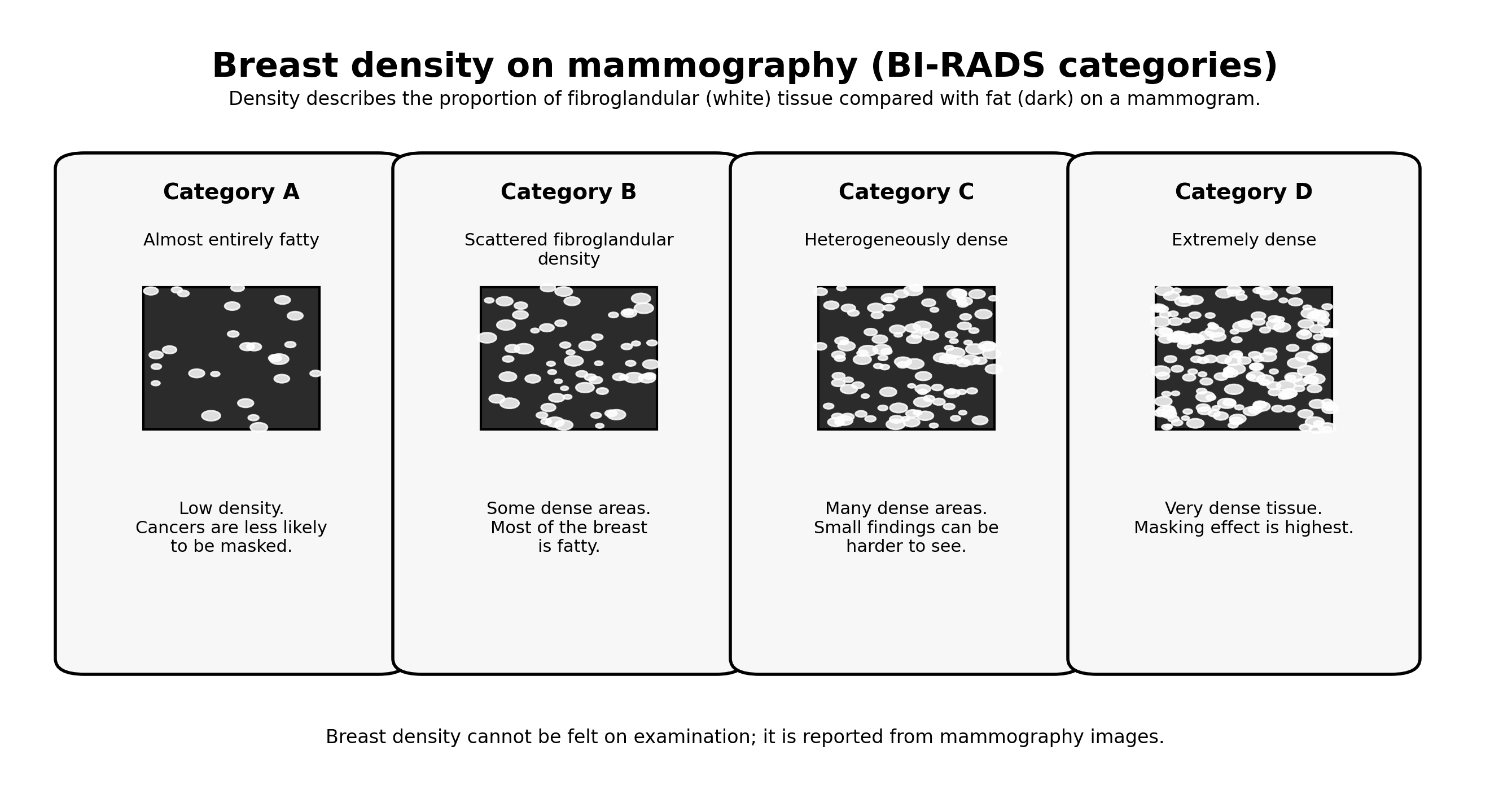
Breast density describes the proportion of fibroglandular tissue (glands and fibrous supporting tissue) compared with fat. On a mammogram, fatty tissue tends to look darker, while fibroglandular tissue appears whiter.
Density is commonly reported using four categories (often referred to as BI-RADS A–D). I include this because it helps patients understand that density is a spectrum rather than a “yes/no” label.
Can I feel breast density?
No. Density is not something you can reliably feel on self-examination or a clinical examination. It is assessed on mammography images.
Does breast density change over time?
It can. Many people find density reduces with age, especially after menopause, but this is variable and influenced by individual factors.
Why dense breasts matter
There are two main reasons density is discussed:
- Masking effect: dense tissue can make it harder to detect small abnormalities on mammography because both dense tissue and many cancers can look white.
- Risk context: higher density is associated with a higher likelihood of developing breast cancer compared with low density. This does not mean you will develop cancer; it simply becomes one piece of your overall risk profile.

Why mammography and ultrasound can play different roles
In practice, the “best” test depends on what question we are trying to answer. I frame it like this: mammography is the overview test (especially for screening), while ultrasound is often the targeted problem-solving test (especially for symptoms).

Role of mammography (including tomosynthesis/DBT where used)
- Primary role: population screening and broad assessment of breast structure.
- Strength: detects calcifications and subtle architectural changes that ultrasound may not show as well.
- Limitation in dense tissue: the masking effect can reduce sensitivity, which is why the overall clinical context matters.
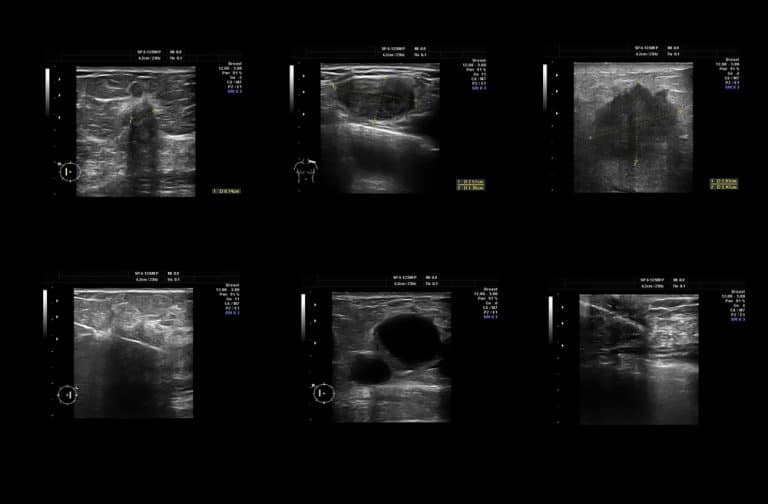
Role of breast ultrasound
- Primary role: targeted assessment of symptoms (for example a lump, focal thickening, a painful area, or nipple discharge).
- Strength in dense breasts: can help characterise focal findings in dense tissue because it is not affected in the same way as mammography.
- Important limitation: ultrasound is not a “replacement” for mammography in screening; it is usually an adjunct or a symptom-led test.
Role of MRI (selected pathways)
MRI is not routinely required for most people. It is typically reserved for higher-risk pathways or for problem-solving when the clinical concern persists despite first-line imaging.
Clinical context: when ultrasound may be added
The most practical way to think about dense breasts is to split it into two situations:
- Screening context: you have no symptoms, but you have been told your breasts are dense.
- Symptom-led context: you have a symptom (for example a new lump, nipple change, blood-stained discharge, focal persistent pain).

If you have symptoms
If you have a new breast symptom, density becomes less important than the symptom itself. In that scenario, I commonly use targeted ultrasound to assess the specific area of concern, and add mammography as appropriate for age and context.
If you have no symptoms
If you are asymptomatic, the decision to add supplemental imaging depends on your overall risk profile (for example family history, genetics, previous breast cancer, or other risk factors), balanced against the possibility of false positives and additional testing.
What I recommend you do if you are told you have dense breasts
- Do not panic: density is common and is a descriptive mammogram finding.
- Stay engaged with screening: mammography remains important even if tissue is dense.
- Assess your risk properly: density is only one factor; risk is the whole picture.
- If you develop symptoms, book assessment promptly: symptom-led imaging is the safest route.
FAQs
Does having dense breasts mean I have cancer?
No. Dense breasts do not mean you have cancer. They describe the tissue composition seen on mammography.
Should everyone with dense breasts have an ultrasound?
Not automatically. Ultrasound is most valuable when there is a symptom to investigate or when you are in a selected higher-risk pathway. The best approach is personalised to your risk and your clinical context.
Can ultrasound miss cancers?
Yes. No imaging test is perfect. Ultrasound is excellent for targeted assessment and characterisation, but it does not replace mammography for screening. In higher-risk contexts, MRI may be considered.
Can breast density be reduced?
Density can change over time, often reducing with age, but it is not something we “treat” directly. The goal is to choose the right imaging pathway for your situation.
Booking note (IUS London)
If you have a new breast symptom (lump, focal thickening, skin or nipple change, or blood-stained discharge), I recommend prompt clinical assessment. If you have been told you have dense breasts and want a structured discussion about the most appropriate imaging in your context, we can guide you toward the right pathway.
Next step: Contact IUS London to book
Content Information
We review all clinical content annually to ensure accuracy. If you notice any outdated information, please contact us at info@iuslondon.co.uk.
About the Author:

Dr. Mohammad Jalaleddin (GMC number: 7729988) is an internationally-trained physician who earned his medical degree from Tishreen University in Syria in 2005. He completed his specialization in diagnostic radiology in 2009, followed by a Master's degree in 2011, which focused on the radiological alterations of bone grafts. Dr. Jalaleddin has worked as a radiologist in various hospitals and clinics, developing significant expertise in ultrasound and MRI scans. He has extensive experience in performing a wide range of ultrasound examinations, including breast, abdominal, pelvic, and vascular studies. In 2017, he moved to the UK and completed the requalification process with the General Medical Council (GMC). Since March 2021, he has been a part of the Imperial College Healthcare NHS Trust. Dr. Jalaleddin is a member of the General Medical Council (GMC) and the British Medical Ultrasound Society (BMUS).